Inside the unconscious brain
New study reveals brain-wave patterns that mark loss of consciousness during anesthesia.
A new study from MIT and Massachusetts General Hospital (MGH) reveals, for the first time, what happens inside the brain as patients lose consciousness during anesthesia.
By monitoring brain activity as patients were given a common anesthetic, the researchers were able to identify a distinctive brain activity pattern that marked the loss of consciousness. This pattern, characterized by very slow oscillation, corresponds to a breakdown of communication between different brain regions, each of which experiences short bursts of activity interrupted by longer silences.
“Within a small area, things can look pretty normal, but because of this periodic silencing, everything gets interrupted every few hundred milliseconds, and that prevents any communication,” says Laura Lewis, a graduate student in MIT’s Department of Brain and Cognitive Sciences (BCS) and one of the lead authors of a paper describing the findings in the Proceedings of the National Academy of Sciences this week.
This pattern may help anesthesiologists to better monitor patients as they receive anesthesia, preventing rare cases where patients awaken during surgery or stop breathing after excessive doses of anesthesia drugs.
“We now finally have an objective physiological signal for measuring when someone’s unconscious under anesthesia,” says Patrick Purdon, an instructor of anesthesia at MGH and Harvard Medical School and senior author on the paper. “Now clinicians will know what to look for in the EEG when they are putting someone under anesthesia.”
Other MIT authors of the PNAS paper are co-lead author Veronica Weiner, a graduate student in BCS, and Emery Brown, professor of brain and cognitive sciences and health sciences and technology at MIT and an anesthesiologist at MGH.
Breakdown of communication
For this study, the researchers focused on propofol, one of the most commonly used anesthesia drugs. Propofol activates receptors found on neurons that are likely to make the neurons less active, but its precise effects on the brain were not known.
The researchers studied epileptic patients who had electrodes implanted in their brains to monitor their seizures, and were undergoing surgery to have the electrodes removed. Loss of consciousness occurred within 40 seconds of propofol administration, and was defined by the moment when patients stopped responding to sounds that were played every four seconds.
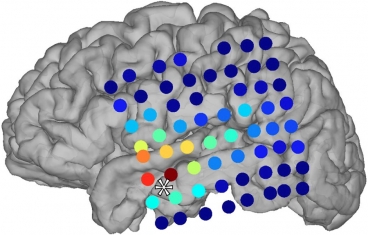
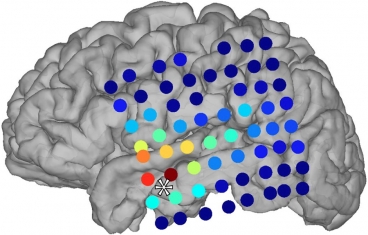
Using two different-sized electrodes, the researchers were able to obtain two different readings of brain activity. The larger electrodes, slightly bigger than a penny, were spaced about a centimeter apart and recorded the overall EEG, or brain-wave pattern.
Smaller electrodes, in an array only 4 millimeters wide, recorded from individual neurons, marking the first time anyone has recorded from individual neurons in human patients as they lost consciousness. Between 50 and 100 electrodes were implanted in each patient, clustered in different regions.
From the large electrodes, the researchers observed that within a couple of seconds of losing consciousness, the brain EEG abruptly took on a pattern of low-frequency oscillation, about one cycle per second. At the same time, the electrodes recording from individual neurons revealed that within localized brain regions, neurons were active for a few hundred milliseconds, then shut off again for a few hundred milliseconds. This “flickering” of activity created the slow oscillation seen in the EEG.
“When one area was active, it was likely that another brain area that it was trying to communicate with was not active. Even when the neurons were on, they still couldn’t send information to other brain regions,” Lewis says.
Michael Avidan, a professor of anesthesiology at Washington University School of Medicine, says the findings are exciting because they offer neurobiological evidence for one of the theories of how the brain gives rise to consciousness. That theory, known as information integration theory, suggests that large-scale brain networks integrate many types of sensory input to generate our overall experience of the world.
When consciousness is lost, “there may still be information coming into the brain, but that information is remaining localized and doesn’t get integrated into a coherent picture,” says Avidan, who was not part of the research team.
Failure of information integration had previously been suggested as a possible mechanism for loss of consciousness, but no one was sure how that might happen. “This finding really narrows it down quite a bit,” Brown says. “It really does, in a very fundamental way, constrain the possibilities of what the mechanisms could be.”
A delicate balance
Patients who receive too little anesthesia risk awakening in the middle of their surgery, while too much drug can cause respiratory problems and even halt breathing. Anesthesiologists must give just the right amount of drugs to keep patients in the appropriate state.
Currently, anesthesiologists monitor anesthesia with recordings that compute an index from the EEG. That index obscures the physiology that can be observed directly in the slow waves.
“What this study says is that you should be looking at raw EEG in order to observe the oscillations and interpret them. If you do that, you have a physiologically linked way to know when someone is unconscious,” Brown says. “We can take this into the operating room today and give better patient care.”
The team is now planning to study what happens to brain activity as consciousness is regained. They have also begun studies of other anesthesia drugs, to see if they produce the same slow oscillation.
“There are many other drugs — based on EEG studies — that seem like they might be producing slow oscillations. But there are other drugs that seem to be doing something totally different,” Purdon says.
The research was funded by an NIH Director’s New Innovator Award, an NIH Director’s Pioneer Award, a fellowship from the Canadian Research Foundation, and the National Institute of Neurological Disorders and Stroke.